Introduction
Chronic obstructive pulmonary disease (COPD) poses a significant challenge to healthcare systems worldwide, necessitating innovative approaches for effective management. Recent research has unveiled a novel Nanoparticle-based immunoantibacterial therapy with the potential to revolutionize COPD treatment.
Nanoparticle Design: Targeted Delivery for Enhanced Efficacy
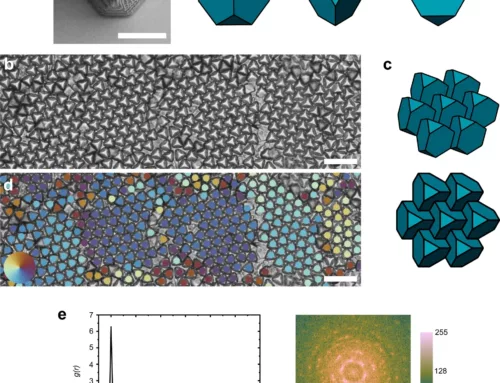
The study, led by scientists from Soochow University, focused on developing polypeptide-gated hollow mesoporous silica nanoparticles (HMSNs) for targeted delivery of antibiotics and immunotherapy directly to the lungs. The nanoparticles’ unique design facilitates penetration of mucus barriers and disruption of bacterial biofilms, enhancing the Nanoparticle-based immunoantibacterial therapy efficacy.
Polypeptide Gate: Controlled Release and Multifunctionality
A key breakthrough lies in the polypeptide gate’s ability to undergo structural transformation in response to acidic pH conditions in bacterial biofilms. This enables precise control over antibiotic release, enhancing bactericidal activity while minimizing systemic exposure. Additionally, the polypeptide gate exhibits multifunctionality, serving as an antibacterial agent, antibiotic adjuvant, and bacterial DNA scavenger, synergistically combating bacterial pathogens and inflammation in COPD.
Safety and Biocompatibility: Promising Preclinical Results
Comprehensive in vivo analyses demonstrate excellent biocompatibility and safety profiles of the nanoparticles, supporting their potential for clinical translation. Hematological, biochemical, and histological assessments underscore the nanoparticles’ safety and efficacy in COPD management.
Therapeutic Efficacy: Restoring Pulmonary Function
In COPD mice models, nanoparticle-based therapy significantly improves pulmonary function, evidenced by enhancements in arterial blood gas parameters and histopathological changes in lung tissues post-treatment. This underscores the therapy’s potential in reversing COPD-related pulmonary dysfunction and promoting lung function recovery.
Clinical Implications and Future Directions
The nanoparticle-based immunoantibacterial therapy represents a paradigm shift in COPD management, offering a targeted and multifunctional approach to address bacterial infection and chronic inflammation. Further research is warranted to optimize nanoparticle design, evaluate long-term safety, and conduct clinical trials to validate efficacy in human subjects, potentially transforming COPD treatment approaches.
Conclusion
The development of nanoparticle-based immunoantibacterial therapy signifies a groundbreaking advancement in COPD management, with the potential to improve clinical outcomes and reduce the burden of this debilitating respiratory condition. With continued research and clinical validation, this innovative strategy holds promise in transforming COPD treatment and enhancing the quality of life for millions affected globally.
Journal reference: Science Advances DOI: 10.1126/sciadv.abd7904